Critical Review of:
Rusin, J; Debell, R. Anthropometrical Considerations for Customizing the Squat Pattern . Personal Training Quarterly, February 2019 Vol 4, Issue 5
- The article can be read in full here - How to Find Your Best Squat Stance
by Brent Brookbush DPT, PT, COMT, MS, PES, CES, H/FS, HMS
Author's Note:
I generally feel that publicly critiquing other credentialed professionals adds to the culture of "trolling", and with that in mind I try to refrain. However, there are certain claims being made in the industry which are supported by little more than opinion, fallacies and the misrepresentation/interpretation of research. This paper falls into that category. In my humble opinion the mistakes made in the paper should have prohibited publication, and the article should be retracted or at the very least amended. Further, the publication of this article should raise some questions regarding the rigor of the editorial process for Personal Training Quarterly.

Summary of Issues:
- This article falsely assumes that structural variations are evenly distributed among the population, rather than respecting normal distribution, or the prevalence of significant structural differences.
- Two studies suggest that roughly 6% of individuals exhibit significant differences.
- Suggesting a protocol for all individuals, when research suggests that a relatively small number of individuals are affected by the issue addressed (hip morphology).
- Assuming correlation where no correlation has been demonstrated.
- There is no evidence to suggest that altering foot placement during a squat would aid in increasing performance or decreasing the risk of injury in individuals with abnormal hip morphology.
- Use of a test/protocol for a purpose it was not intended.
- The use of the "Quadrant Test" in this article differs greatly from the tests original intent, resulting in a lack of evidence of validity or reliability.
- Suggesting extreme action for small variations.
- Based on the images in the article, 20º - 70º of turn-out (based on images in article) is recommended to compensate for differences in hip morphology between 5º - 15º.
- Further, how would both anteversion and retroversion be addressed by using a wider/turned-out stance?
- There are a number of fallacious arguments used to "sell" the need for consideration - appeal to authority, argument to the people, appeal to ignorance, appeal to intimidation (large words), straw-man arguments.
- There is no mention of validated, reliable, research supported methods for addressing the mobility issues alluded to in the article. That is, there is no mention of techniques that may be used to improve lower extremity alignment, hip mobility, ankle mobility, etc., reducing the need to alter foot placement.
- This may be evidence of cherry-picking and/or confirmation bias. The scientific method is dependent on conclusions following the gathering of data. The authors may be guilty of coming to a conclusion and then looking for research to support it.
Critique:Italicized text is quoted from Rusin and Debell (2019)
Note: Key paragraphs have been selected with the intent of "stream-lining" the review. Whole paragraphs were pulled from the article to ensure that sentences/statements were presented in context. |
DEBUNKING DEEPLY ROOTED SQUAT DOGMA
…..
As we gain more insights into the unique anatomical, biomechanical, and neuromuscular variables between individuals, the need to customize a squat pattern according to an individual’s specific needs instead of their theoretical sport or goal set has become apparent. If people are all built differently how could they all squat the same?
- The research cited in this article does not support the notion that a large variety of anatomical differences occurs in the gross majority of the population.
- The need to individualize a squat has become apparent to who?
- There is no evidence to suggest that individualizing a squat will have any positive effect on any individual.
- The statement "instead of their theoretical sport or goal set" contradicts the principle Specific Adaptation to Imposed Demands (SAID). This assertion contradicts a principle that is based on a significant body of research. Although there may be room to refine the SAID principle, inserting such a significant contrary notion is not appropriate. This should be addressed in a separate paper. It is time to throw away the one size fits all dogmatic approach to squatting.
- "One size fits all, dogmatic approach" is language used to set-up a "straw man" argument. That is, this position is not actually proposed by any specific person or group. They may be trying to imply that a reference model of "ideal form" (based on normative data and research) is dogmatic; however, a reference model and a dogmatic approach are not one in the same.
- Further, this statement alone leads to a slippery slope argument - If a standard reference model of form does not exist, then what is "good form?" What does "individualized" mean? Does that mean everyone should squat how they are comfortable? Is the implication that 100s of studies on compensation, restriction, altered motor patterns and injury are wrong? Etc.
Outlined below is a method to help determine an individual’s preferred squatting foot position, setup, and depth based on their unique hip anthropometrics for smarter, safer and more optimized squatting.
- It is irresponsible to state that an untested methodology is smarter, safer or optimized without any 3rd party evidence. The reader has no reason to believe that these methods are safer or improve performance (And I am not sure how you would measure "smarter"). Further, this critical review highlights several assumptions and fallacies that the methodology is built on.
HIP VARIATION AND SQUATTING
…The anatomical differences from person to person of the bony anatomy of the hip cannot be ignored when finding the best squat stance for the longevity of the athlete. The differences in hip anatomy will affect the ability of an athlete to squat in a certain stance. The main considerations for bony anatomical variation of the hip are:
- Missing research (support):
- There is no study suggesting that there is a high rate of statistically significant differences in hip morphology.
- There is no study to show that changing squat stance would decrease the risk of injury or increase performance if a difference in hip morphology did exist.
- There is no study to imply a relationship between the degrees of anteversion or retroversion and the degrees of foot/hip turn-out needed to ensure "optimal motion" of the hip (decreased risk, increased performance).
- There is no research to suggest a correlation exists between hip anatomy and foot placement. There are a number of angles that exist between the hip and foot that may compensate for altered hip morphology during development. For example, a 5° difference in anteversion may be easily compensated for by a 1° change (which is within normal variation) in these other angles.
- Talar neck angle
- Angle of axis of the ankle
- Tibial torsion
- Genu valgum angle
- Femoral angle of inclination
- Q-angle
- Alternatively there is research that correlates altered alignment with injury (assessed during a squat), and several studies that demonstrate alignment issues may increase risk of future injury (alluding to causation).
HIP VARIATION AND SQUATTING (continued)
Since both the head of the femur and hip socket can have variations in version (forward/backward orientation), the sum version should be considered. The McKibbin Instability Index is used to sum the versions and may be predictive of hip issues with squatting (4).
- (4). Original Citation: Fabricant, P. D., Fields, K. G., Taylor, S. A., Magennis, E., Bedi, A., & Kelly, B. T. (2015). The effect of femoral and acetabular version on clinical outcomes after arthroscopic femoroacetabular impingement surgery. JBJS, 97(7), 537-543. - Abstract
- This citation is very misrepresented:
- "The McKibbin Instability Index is used to sum the versions and may be predictive of hip issues with squatting (4)." This statement is not at all supported by the findings of this study. The study itself demonstrates a lack of predictive power of the McKibbin Instability Index for post surgical outcomes, and does not mention the squat at all.
- Quoted from the study: "“We did not find any associations between the McKibbin index and any patient-reported outcomes.”
- Further, this is a study on outcomes post hip surgery. It is likely that a population of individuals who were candidates for hip surgery have a higher rate of "abnormal structure" than the general population. Further, what is the relevance between post-surgical patients and the generally healthy population working with personal trainers? This is what is referred to as "over-generalization" or a lack of relevance.
- "The McKibbin Instability Index is used to sum the versions and may be predictive of hip issues with squatting (4)." This statement is not at all supported by the findings of this study. The study itself demonstrates a lack of predictive power of the McKibbin Instability Index for post surgical outcomes, and does not mention the squat at all.
WHAT IS FEMORAL VERSION?
- This section of the paper defines and illustrates anteverion and retroversion. The author's descriptions are similar to those published in various texts.
- From: Hip (Pelvifemoral) Joint (by the Bookbush Institute)
- Femoral Torsion (transverse plane) (1, 2):
- Normal Range: 8º-15º
- Anteversion: > 15 - 20º (may present with "toe in" posture)
- Retroversion: < 8º (may present with "toe out" posture)
- Donald A. Neumann, “Kinesiology of the Musculoskeletal System: Foundations of Rehabilitation – 2nd Edition” © 2012 Mosby, Inc.
- Cynthia C. Norkin, Pamela K. Levangie, Joint Structure and Function: A Comprehensive Analysis: Fifth Edition © 2011 F.A. Davis Company
- Femoral Torsion (transverse plane) (1, 2):
ANATOMICAL VARIATIONS – ACETABULUM (Pictures)
Sample picture:

- This section of the paper is very misleading. This section displays a series of photos that depict pelvis and femurs that were obviously hand selected to demonstrate differences in anatomy. Citing extremes as if they represent the norm is a logical fallacy. This would be the equivalent of selecting a male who is 3'6" with achondroplasia and a 7'1" basketball player, and presenting the two as examples of normal variants in height for men. Although these heights exist, we cannot call them "normal" variants. A little digging, and a cursory understanding of normal distributions (bell curves), and you will soon find that nearly 70% of men are between 5'7" and 6'1" and 96% are between 5'4" and 6'4". In fact, the 2 heights selected above would likely represent less than 1% of 1% of the population.
- Citing extremes as if they represent the norm is one of the glaring fallacies (and mistake) proposed in this paper. Because we know the normative distribution of height we can assume things like a 3-foot-high counter-top is comfortable for the gross majority of individuals. We know that a small percentage will find a 3-foot-high counter-tops uncomfortable, and we know an even smaller percentage of the population will likely need custom counter-tops because 3' counter-tops are not even manageable (poor Shaq).
- In the same way, a reference model of the squat form can be developed, with an understanding that a small portion of the population will need to make minor modifications (5-7%, less than 1 standard deviation), and only a very, very, very small percentage (0.1 - 0.5% standard deviations) will need to make significant modifications (like those recommended at the end of this article). The idea that everyone is significantly different is just not true.
Version of the hip can vary by region of the world (3,12) and by gender (1,5). In one study, the average Caucasian male was shown to have seven degrees of anteversion (range -2 to 35 degrees) and the average Chinese male had 14 degrees of anteversion (range -4 to 36 degrees) (5). In a study on femoral version in populations across ethnicities, Caucasian males were shown to have retroversion at a rate of 24.1%, African American males at a rate of 15.1%, and all ethnicities of females at 14.3% (6). With the known variations in hip morphology, an assessment is indicated to place people in the proper squat stance for their body.
- This entire paragraph ignores the results of the research studies, means, distribution and prevalence. The studies either demonstrate no significant differences or small significant differences in MEAN anterversion/retroversion. Note, there is only one study that shows a mean outside of the range of 18 - 23°, and that is the study by Hoaglund et al. (5) demonstrating 8 - 14°. Comparing the results of two studies is problematic, as the comparison is indirect, and if differences in measuring methodologies exist then comparison may be impossible. (Given these small differences, how does the author justify 45° and 70° of turn-out as recommended later in this article?). More often then not, statistics like these can be represented by a bell curve.
- The numbers here actually get pretty confusing as some studies cited are discussing "anteverion" or "retroverion" from a reference of normal version angle, and other studies are adding the normal version to the additional angle of anteversion and retroversion and reporting it as one number. All studies report the mean, however, the data sets for several studies are not large enough to imply an accurate representation of the distribution curve. Further, some of the studies are using cadavers which adds confounding variables regarding nutrition, activity and health status of individuals who may have developed 50 years ago when resources in various countries were not as equatable as they are now. (Many of our bone angles are the result of weight bearing in early childhood development).
- Note, the two studies that investigated prevalence of anomalies (Koerner et al. and Ezoe et al.) demonstrated roughly 6% exhibited differences significant enough to be considered "retroversion".
- This is the best evidence currently available, and does not support the notion that "variation" is equally represented across all individuals. As mentioned above, this implies that a small subset of individuals may need to make minor modification from a reference model of good form.
- Cited studies and selected quotes:
- (3.) Eckhoff, D. G., Kramer, R. C., Watkins, J. J., Alongi, C. A., & Van Gerven, D. P. (1994). Variation in femoral anteversion. Clinical Anatomy: The Official Journal of the American Association of Clinical Anatomists and the British Association of Clinical Anatomists, 7(2), 72-75.
- Quoted from Study: Variation in femoral anteversion in an adult African skeletal population is examined in this study. Variation is measured in reference to population, gender, and side of the extremity (right vs. left). This study demonstrates greater average anteversion (19°) and a significant right‐left variation (21 vs. 17) when compared to previously reported Caucasian and Oriental populations.
- (12.) Saikia, K, Bhuyan, S, and Rongphar, R. Anthropometric study of the hip joint in Northeastern region population with computed tomography scan. Indian Journal of Orthopaedics 42(3): 260, 2008.
- Quoted from Study: Results: The mean parameters observed were as follows: acetabular angle 39.2°, centre edge angle 32.7°, neck shaft angle 139.5°, acetabular version 18.2°, femoral neck anteversion 20.4°, acetabular depth 2.5 cm and joint space width 4.5 mm.
- (1.) Atkinson, H. D., Johal, K. S., Willis-Owen, C., Zadow, S., & Oakeshott, R. D. (2010). Differences in hip morphology between the sexes in patients undergoing hip resurfacing. Journal of orthopaedic surgery and research, 5(1), 76.
- Quoted from study: (Note: Again, this was a study on surgical candidates which may inflate variation numbers). There were no sex differences in femoral torsion/anteversion, femoral neck angle and acetabular inclination. Males had a mean femoral torsion/anteversion of 8 degrees (range -5 to 26 degrees), a mean femoral neck angle of 129 degrees (range 119 to 138 degrees) and a mean acetabular inclination of 55 degrees (range 40 to 86 degrees). Females had a mean femoral torsion/anteversion of 9 degrees (range -2 to 31 degrees), a mean femoral neck angle of 128 degrees (range 121 to 138) and a mean acetabular inclination of 57 degrees (range 44 to 80 degrees). Females had a significantly greater acetabular version of 23 degrees (range 10 to 53) compared with 18 degrees in males (range 7 to 46 degrees (p = 0.02) and males had a significantly greater femoral offset of 55 mm (range 42 to 68 mm) compared with 48 mm (range 37 to 57 mm) in females (p = 0.00).
- (5) Hoaglund, F. T., & Low, W. D. (1980). Anatomy of the femoral neck and head, with comparative data from Caucasians and Hong Kong Chinese. Clinical orthopaedics and related research, (152), 10-16.
- The femoral neck is anteverted from the transcondylar plane on the average 8 degrees in the adult. In measurements that we made of femora from cadavers of Caucasians, the anteversion angle averaged 7.0 degrees in males (range, --2 degrees to 35 degrees) and 10.0 degrees in females (range, -2 degrees to 25 degrees). Using similar techniques on cadavers of Hong Kong Chinese, we found that the average in males was 14.0 degrees (range, --4 degrees to 36 degrees) and 16.0 degrees in females (range, 7 degrees to 28 degrees).
- (6) Koerner, J. D., Patel, N. M., Yoon, R. S., Sirkin, M. S., Reilly, M. C., & Liporace, F. A. (2013). Femoral version of the general population: does “normal” vary by gender or ethnicity?. Journal of orthopaedic trauma, 27(6), 308-311.
- Conclusions: Although there may not be a significant difference in average femoral version between ethnic and gender groups, retroversion is relatively common, and retroversion .108 was observed in nearly 6% of the African American population. This may have important implications in proper alignment restoration and successful clinical outcomes after intramedullary nailing of femur fractures.
- Additional study not included in the article
- Ezoe, M., Naito, M., Inque, T. (2006). The prevalence of acetabular retroversion among various disorders of the hip. The Journal of Bone and Joint Surgery. 88A (2). 372-379
- Quoted from the study: The prevalence of acetabular retroversion was 6% (seven of 112 hips) in the normal group
FUNCTIONAL QUADRANT TESTING TO DETERMINE APPROPRIATE SQUAT STANCE
In order to objectively assess all unique variables of both the femur and acetabulum interplay as a functioning unit that can be scaled up with the squat pattern, a standard orthopedic assessment called the quadrant test, also known as the hip scour, test can be used (2).
- (2). Cook, CE, and Hegedus, EJ. Orthopedic Physical Examination: An Evidence Based Approach. Upper Saddle River, NJ: Pearson Prentice Hall; 2008.
- Note: Authors use an outdated version of this textbook. Current version:
- Cook, C. E., & Hegedus, E. (2012). Orthopedic physical examination tests: an evidence-based approach. Pearson Higher Ed.
- Note: Authors use an outdated version of this textbook. Current version:
- The text by Cook and Hegedus is excellent, with a summary of nearly all available research on specificity, sensitivity, reliability and quantitative utility score for 100s of special tests. Only two studies were cited by Cook et al. for the "Quadrant" or "Hip Scour" test with no mention of accuracy, and only one study demonstrating reliability.
- Cliborne, A. V., Wainner, R. S., Rhon, D. I., Judd, C. D., Fee, T. T., Matekel, R. L., & Whitman, J. M. (2004). Clinical hip tests and a functional squat test in patients with knee osteoarthritis: reliability, prevalence of positive test findings, and short-term response to hip mobilization. Journal of Orthopaedic & Sports Physical Therapy, 34(11), 676-685.
- Mitchell, B., McCrory, P., Brukner, P., O'Donnell, J., Colson, E., & Howells, R. (2003). Hip joint pathology: clinical presentation and correlation between magnetic resonance arthrography, ultrasound, and arthroscopic findings in 25 consecutive cases. Clinical journal of sport medicine, 13(3), 152-156.
- A more recent study showed the "quadrant test" was less accurate than other special tests that may be used for diagnosing hip impingement syndrome .
- Maslowski, E., Sullivan, W., Forster Harwood, J., Gonzalez, P., Kaufman, M., Vidal, A., & Akuthota, V. (2010). The diagnostic validity of hip provocation maneuvers to detect intra‐articular hip pathology. Pm&r, 2(3), 174-181.
This test has been utilized for decades in orthopedic practice to manually assess and diagnose the presence and/or location of a hip labral tear, among other unique pathologies such as degeneration, femoral-acetabular impingement, and avascular necrosis of this region (10).
- (10.) Original Ctitation: Manning, C., & Hudson, Z. (2009). Comparison of hip joint range of motion in professional youth and senior team footballers with age-matched controls: an indication of early degenerative change?. Physical Therapy in Sport, 10(1), 25-29.
- This findings of the study referenced have nothing to do with the intent of the statement made by the authors. In this study a group of "footballers" was assessed for signs of early degenerative changes of the hip using a group of common orthopedic tests including the "quadrant test". The differences noted in the group of football players did not include any differences determined by the "quadrant test". If anything, this study shows that the "quadrant test" lacks sensitivity; is not a good test for identifying risk factors.
The goal for administering this assessment is not to medically diagnose pain or dysfunction, but rather to use the key positions and properties which make this test extremely reliable to gain an appreciation for the femoral acetabular joint’s shape, size, and movement capacity at the deepest joint level minus restrictions from local soft tissue structures.
- This test was developed with the intent of diagnosing labral tears, or potentially hip impingement syndrome. Using the test for other purposes is not validated. That is, there is no evidence to suggest the quadrant test would be effective for testing any other issue. Soft tissue structures like the posterior capsule, piriformis , posterior rotators of the hip , and posterior head of adductor magnus are all stretched to end range (or close to end range) in this position and are very likely to restrict motion. The idea that joint shape and size could be determined with this test is bordering on ridiculous. How could any professional differentiate between small variations (millimeters) in bones surfaces and the interaction of both intra-articular structures and the soft tissues mentioned above.
- Further the statement about "extremely reliable" is completely unfounded. Reliability is a mathematical representation of the agreement between testers and/or the test performed multiple times by the same tester. Reliability is not something that can simply be assumed, especially considering the use of the test in this article has not been validated.
Positioning your client down in the supine position allows full support of the spine and pelvis in a neutral position, which is of pivotal importance when testing in a reliable and repeatable manner. As with any standardized testing position, the presence of compensation patterns at any segment in the body other than that being tested can lead to false positives and unreliable data collection that can make it more difficult to reliably scale it up the squat pattern based on the key measurements taken. Ensure that the lower extremity on the testing side is the only aspect of the body moving to avoid compensations from the pelvis, spine, or opposite side extremity. From this position, degrees of hip flexion, external rotation, and abduction occurring synergistically will be tested in order to maximize a pain-free hip flexion angle which will represent the theoretical glass ceiling on squat depth that the hip joint itself is able to display with motor control taken out of the equation.
- Although some of this paragraph includes correct information, it is applied to a test that is being used in a way that has not been validated and is likely unreliable. A reliable method for determining hip range of motion (ROM) is goniometry .
- Not really sure why the authors felt it necessary to invent a method, when validated, reliable methods for assessing ROM exist.
- Note: The assertion that hip range of motion effects squat form can be supported by the evidence. Further, research also demonstrates that changes in alignment and range of motion are predictive of future injury. Research does NOT support that these changes in range of motion and alignment are due to altered hip morphology, or that they can be assessed as described by the authors.
- Research has demonstrated the validity and reliability of the Overhead Squat Assessment
- An assessment that looks for specific deviations in alignment from a reference (ideal) model (including foot turn-out and knees bow-out).
- Range of motion can be reliably assessed via goniometry
- Several techniques and methodologies have demonstrated efficacy for increasing extensibility of soft tissues , reducing abnormal joint stiffness , improving activity of under-active muscles , and even reducing the presence of signs on the Overhead Squat Assessment associated with risk of future injury.
- Selected research on these topics listed below
By moving the hip in and out of these windows of motion with the leg reaching terminal knee to chest position with rotary planes also involved, centration of the hip joint can occur. Centration can be defined as maximizing the surface area contact of any joint, in this case, the femoral head into the acetabulum of the pelvis. Increased joint centration can increase the activation of intrinsic stabilizers of the region, and also allow optimal length tension relationship of some bigger secondary dynamic stabilizers, such as the gluteal and adductor group, in order to more optimally position for biomechanical success in the squat pattern. This also allows stronger neuromuscular recruitment and coordination of this compound movement pattern centered around the hip complex.
- This is not the definition of centration, which generally refers to arthorkinematic motion maintaing congruence between the center of two joint surfaces (axis of rotation). The authors seem to be confusing the terms centration and "close-pack" position.
- The rest of the paragraph is conjecture. Optimal length/tension refers to the optimal length of muscles, the gluteal and adductor group are not often referred to as "dynamic stabilizers," and there is no evidence that the protocol the authors are referring to has any effect on neuromuscular recruitment. This entire paragraph screams "argumentum ad verbusum" (essentially, intimidation with big words).
It is important to note that this assessment takes practice, repetitions, and experience to reliably administer, especially for the goals of grading it up into the squat pattern.
- This might be true if the authors were not referring to an assessment that has not been validated, and is being used for an issue that only exists in a small percentage of the population. A study on negative and positive predictive values would likely render this assessment protocol ineffective.
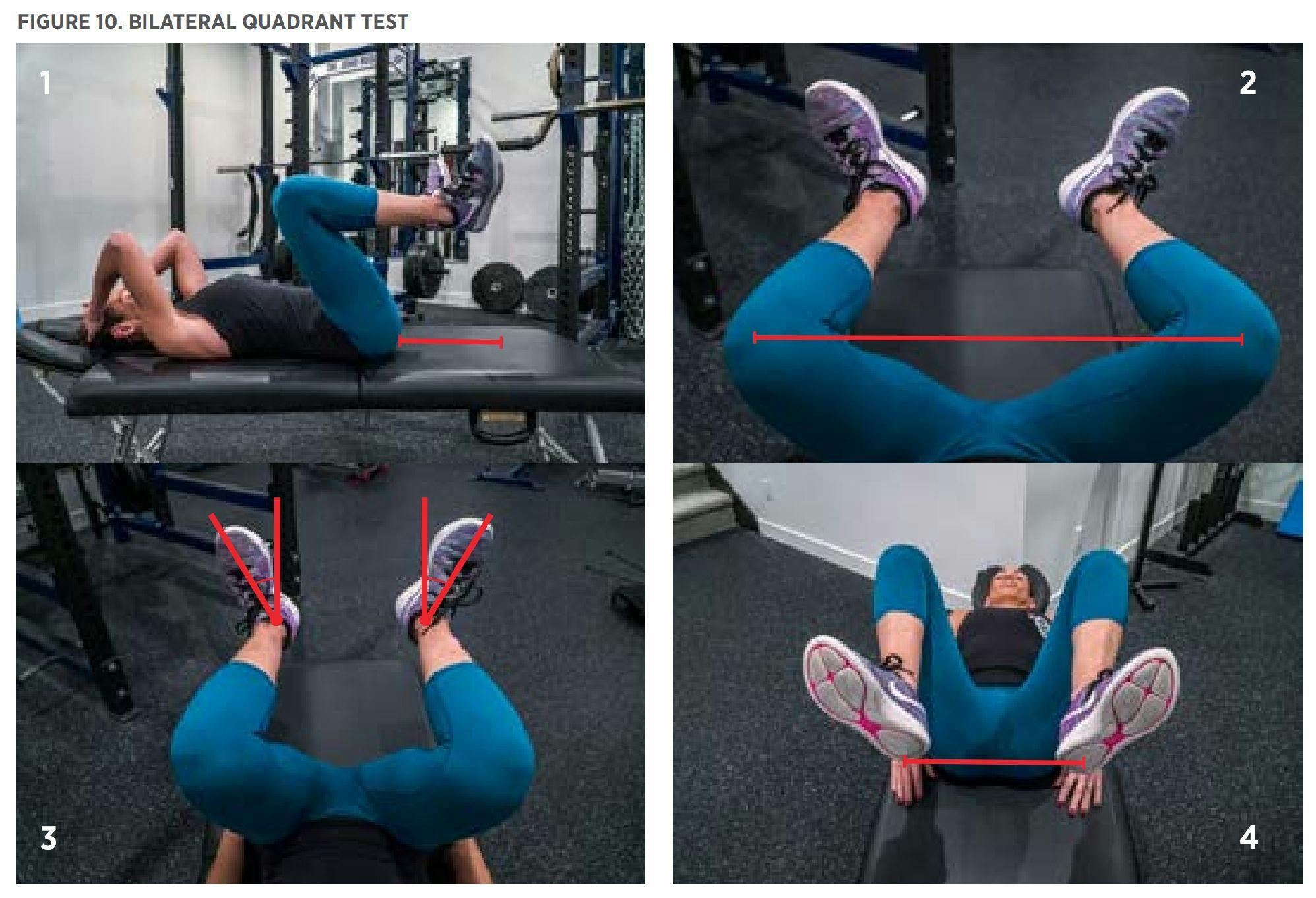
Once optimal hip position on one side of the body is determined, cue your client to hold their knee in that position while you repeat the assessment for the opposite side. Once both hips have been assessed and your client is holding both in place with cues such as “glutes flexing” and “toes up,” it is time to take measurements and record your data.
The four measurements are:
- Buttocks-to-floor distance
- Distance between knee caps from mid-patellar line
- Foot abduction angle from foot’s midline
- Distance between heels at mid-calcaneal line
Utilizing this data, especially the mid-calcaneal foot width and the foot abduction (toe out) angle, we can scale this squat setup into the standing position starting with these measurements. Note that the mid patellar width and the buttocks-to-floor distance may not be instantly translated into the standing position due to a lack of motor control skill set in this new stance. This will be the time to coach around these positions with the goal of reaching the theoretical buttocks-to-floor distance and knee cap width distance at terminal authentic end range of motion.
- Obviously this protocol is unique to the authors. Innovation is important; however, because this assessment is built on a false assumption of equal distribution, using an assessment that has not been validated, looking for outcomes that have no correlation to hip morphology… it seems very unlikely that this protocol is useful. Pointing out a couple obvious flaws:
- Hip flexion range of motion may increase with abduction and external rotation in individuals with normal hip morphology.
- Soft tissue restriction is at least as likely to effect this protocol as hip morphology (and soft tissue restriction can be resolved using various techniques).
- Research has demonstrated that feet turn out and knee varus are correlated with pain and dysfunction.
- The amount of turn-out demonstrated in these photos far exceeds even the most extreme examples of variations in the studies above.
SIMPLE APPLICABILITY OF SQUAT STANCE CUSTOMIZATION
Given the results of the quadrant tests previously described, there are two main variables that can be altered in a squat stance to maximize athlete comfort, depth, and proper execution of the exercise. The first variable in squat stance is width. After evaluating with the quadrant test, you will find that maximal hip flexion is achieved in some amount of hip abduction vs. adduction before lumbar flexion occurs, which correlates to the mid-patellar distance and distance between heels at the midcalcaneal line. If maximal hip flexion is achieved with relatively more hip abduction, a wider squat stance may be more ideal for that athlete, depending on other factors, such as limb length, torso length, and ankle dorsiflexion range of motion (9). If ankle mobility is limited, a wider stance may be necessary to prevent the center of mass from being too far behind the base of support (8).
- This paragraph is simply explaining the adoption of the feet and knee width found during the assessment protocol described above. Same errors in logic apply.
- The citations used here and the additional citation demonstrate that stance width effects the amount of ankle dorsiflexion, hip flexion and "forward lean" necessary to perform a squat (to parallel or lower). Note, the findings of these studies do not imply that stance width has any correlation with increased performance or reduced risk of injury. Lorenzetti et al. suggest that extremes stance widths should be avoided, which is reasonable. The question I have to ask, is why not attempt to address limits in ankle dorsiflexion, hip flexion or core stability before modifying alignment? Especially in consideration of the chance that alignment may alter motor unit recruitment, increase varus/valgus stress, and potentially lead to injury (see studies listed below).
- (8) Lahti, J., Hegyi, A., Vigotsky, A. D., & Ahtiainen, J. P. (2019). Effects of barbell back squat stance width on sagittal and frontal hip and knee kinetics. Scandinavian journal of medicine & science in sports, 29(1), 44-54.
- Quoted from study: At femur parallel, stance width manipulation in the barbell back squat may provide substantial differences in biomechanical stimulus in both the sagittal plane and the frontal plane. In certain contexts, these differences may have clinically relevant longitudinal implications, from both a performance and a injury prevention standpoint, which are discussed.
- (9) Lorenzetti, S., Ostermann, M., Zeidler, F., Zimmer, P., Jentsch, L., List, R., … & Schellenberg, F. (2018). How to squat? Effects of various stance widths, foot placement angles and level of experience on knee, hip and trunk motion and loading. BMC Sports Science, Medicine and Rehabilitation, 10(1), 14.
- Quoted from study: Suitable stance width and foot placement angles should be chosen according to the targeted joint moments. In order to avoid injury, special care should be taken in extreme positions (narrow stand-42° and wide stance-0°) where large knee and hips joint moments were observed.
- (Additional study with congruent findings) Demers, E., Pendenza, J., Radevich, V., & Preuss, R. (2018). The Effect of Stance Width and Anthropometrics on Joint Range of Motion in the Lower Extremities during a Back Squat. International journal of exercise science, 11(1), 764.
- Odd that the authors did not cite this study - "ANOVA comparison of joint angles for the three stance widths, at 10° intervals of thigh orientation during the squat, indicated that joint angles tended to be larger when stance width was narrower, with the most significant effects on ankle dorsiflexion. A greater trunk/thigh length ratio (relatively long trunk) also tended to be associated with lower ankle and knee angles, while a greater thigh/shank length ratio (relatively long thigh) tended to be associated with higher ankle and knee angles, for the two narrower stance widths. The most practical implication of our findings is that individuals with limited ankle dorsiflexion, or with particularly long legs / thighs, may benefit from a wider stance width when squatting."
- Based on available research I would suggest addressing hip and ankle impairment before modifying alignment during exercise.
- (8) Lahti, J., Hegyi, A., Vigotsky, A. D., & Ahtiainen, J. P. (2019). Effects of barbell back squat stance width on sagittal and frontal hip and knee kinetics. Scandinavian journal of medicine & science in sports, 29(1), 44-54.
Generally, the more retroverted an athlete’s hips, the more toe out they will need to be in the squat, and the more external rotation they will have during the quadrant test to achieve maximal flexion. You will see this as an increased foot abduction angle. For an athlete with more anteverted hips, a relatively more toed forward stance may work better for them (depending on other anatomical variables) in the squat. They will also likely need less hip external rotation to achieve maximal flexion in the quadrant test. You will see this as less foot abduction angle. Testing a combination of stance widths with varying angles of toe out is the best method to determine optimal squat stance after performing the quadrant test, starting with the stance determined by the data acquired in the quadrant test.
- How do the authors know that hips are retroverted or anteverted? Do they have MRIs for eyes? This is another assumption being made by the authors that the comfortable stance width is correlated with hip morphology.
- Even the two studies cited comparing stance width make no mention of hip morphology, and instead report altered hip flexion, dorsiflexion and torso angle.
- Given relatively small number of individuals with retroversion (as cited above)… Would it be more likely that foot position compensates for structural issues, or flexibility issues? Note, mobility issues could be addressed with release, mobilization, stretching and corrective exercise.
End Note from Brookbush:
I have done my very best to remain objective and educational in this review. It is not my intent to personally attack or offend. My hope is that this and other critical reviews will help steer the human movement profession toward evidence-based practice, scientific objectivity and an integrated, outcome driven approach. If you feel any of the statements above are unfair, personal or misstated please leave your critiques in the comments box below. One of the wonderful advantages of online publication is documents can be continually and instantly refined. It is convention that the original authors of academic papers are given the "right of last word". I will respect this convention if Personal Training Quarterly decides to publish this review, and the authors wish to write a rebuttal or amendment.
Keep reading and learning; everyday if possible.
Sincerely,
Dr. B2
Summary of Issues (Mentioned above)
- This article falsely assumes that structural variations are evenly distributed among the population, rather than respecting normal distribution, or the prevalence of significant structural differences.
- Two studies suggest that roughly 6% of individuals exhibit significant differences.
- Suggesting a protocol for all individuals, when research suggests that a relatively small number of individuals are affected by the issue addressed (hip morphology).
- Assuming correlation where no correlation has been demonstrated.
- There is no evidence to suggest that altering foot placement during a squat would aid in increasing performance or decreasing the risk of injury in individuals with abnormal hip morphology.
- Use of a test/protocol for a purpose it was not intended.
- The use of the "Quadrant Test" in this article differs greatly from the tests original intent, resulting in a lack of evidence of validity or reliability.
- Suggesting extreme action for small variations.
- Based on the images in the article, 20º - 70º of turn-out (based on images in article) is recommended to compensate for differences in hip morphology between 5º - 15º.
- There a number of fallacious arguments used to "sell" the need for consideration (appeal to authority, argument to the people, appeal to ignorance, appeal to intimidation (large words), straw-man arguments)
- There is no mention of validated, reliable, research supported methods for addressing the issues alluded to in the article including. That is, there is no mention of techniques that may be used to improve lower extremity alignment, hip mobility, ankle mobility, etc., reducing the need to alter foot placement.
- This may be evidence of cherry-picking and/or confirmation bias. The scientific method is dependent on conclusions following the gathering of data. The authors may be guilty of coming to a conclusion and then looking for research to support it.
Selected Research:
Citations pulled from the bibliographies of:
- Overhead Squat Assessment: Signs of Dysfunction
- Lower Extremity Dysfunction (LED)
- Lumbo Pelvic Hip Complex Dysfunction (LPHCD)
Note: Feet Turn Out and Knees Bow Out are highlighted, as this is the recommended intervention suggested by the authors. The research suggests that these changes in alignment are also correlated with pain and injury.
Overhead Squat Assessment and Reliability:
- Hewett, T. E., Myer, G. D., Ford, K. R., Heidt, R. S., Colosimo, A. J., McLean, S. G., & Succop, P. (2005). Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes A prospective study. The American journal of sports medicine, 33(4), 492-501.
- Buckley BD, Thigpen CA, Joyce CJ, Bohres SM Padua DA. Knee and hip kinematics during a double leg squat predict knee and hip kinematics at initial contact of a jump landing task. J athl Train 2007;42:S81
- Vesci BJ, PAdua DA, Bell DR Strickland LJ, Guskiewicz KM, Hirth CJ. Influence of hip muscle strength, flexibility of hip and ankle musculature, and hip muscle activation on dynamic knee valgus motion during a double-legged squat. J Athl Train 2007; 42:S83
- Gribble, P. A., & Robinson, R. H. (2009). Alterations in knee kinematics and dynamic stability associated with chronic ankle instability. Journal of Athletic Training, 44(4), 350-355.
- Trimble, M. H., Bishop, M. D., Buckley, B. D., Fields, L. C., & Rozea, G. D. (2002). The relationship between clinical measurements of lower extremity posture and tibial translation. Clinical Biomechanics, 17(4), 286-290.
- Mauntel, T. C., Post, E. G., Padua, D. A., & Bell, D. R. (2015). Sex differences during an overhead squat assessment. Journal of applied biomechanics, 31(4), 244-249.
- Noda, T., & Verscheure, S. (2009). Individual goniometric measurements correlated with observations of the deep overhead squat. Athletic Training and Sports Health Care, 1(3), 114-119.
- Bell, D. R., Padua, D. A., & Clark, M. A. (2008). Muscle strength and flexibility characteristics of people displaying excessive medial knee displacement. Archives of physical medicine and rehabilitation, 89(7), 1323-1328.
- Eckard, T., Padua, D., Mauntel, T., Frank, B., Pietrosimone, L., Begalle, R., … & Kucera, K. (2018). Association between double-leg squat and single-leg squat performance and injury incidence among incoming NCAA Division I athletes: A prospective cohort study. Physical Therapy in Sport, 34, 192-200.
Correlation Between Injury and Altered Alignment:
Loss of Dorsiflexion
- Vesci BJ, PAdua DA, Bell DR Strickland LJ, Guskiewicz KM, Hirth CJ. Influence of hip muscle strength, flexibility of hip and ankle musculature, and hip muscle activation on dynamic knee valgus motion during a double-legged squat. J Athl Train 2007; 42:S83
- Gribble, P. A., & Robinson, R. H. (2009). Alterations in knee kinematics and dynamic stability associated with chronic ankle instability. Journal of Athletic Training, 44(4), 350-355.
- Trimble, M. H., Bishop, M. D., Buckley, B. D., Fields, L. C., & Rozea, G. D. (2002). The relationship between clinical measurements of lower extremity posture and tibial translation. Clinical Biomechanics, 17(4), 286-290.
- Bell, D. R., Padua, D. A., & Clark, M. A. (2008). Muscle strength and flexibility characteristics of people displaying excessive medial knee displacement. Archives of physical medicine and rehabilitation, 89(7), 1323-1328.
- Michael RH, Holder LE: The soleus syndrome a cause of medial tibial stress (shin splints). Am J Sports Med 13:87-94 1985
- Souza, T. R., Pinto, R. Z., Trede, R. G., Kirkwood, R. N., & Fonseca, S. T. (2010). Temporal couplings between rearfoot–shank complex and hip joint during walking. Clinical biomechanics, 25(7), 745-748 ‘
- Padua, D. A., Bell, D. R., & Clark, M. A. (2012). Neuromuscular characteristics of individuals displaying excessive medial knee displacement. Journal of athletic training, 47(5), 525.
- Macrum et al. Effect of limiting ankle-dorsiflexion range of motion on lower extremity kinematics and muscle-activation patterns during a squat. Journal of Sport Rehabilitation, 2012, 21, Pg 144-150 .
- Mauntel, T., Begalle, R., Cram, T., Frank, B., Hirth, C., Blackburn, T., & Padua, D. (2013). The effects of lower extremity muscle activation and passive range of motion on single leg squat performance. Journal Of Strength And Conditioning Research / National Strength & Conditioning Association, 27(7), 1813-1823
Feet Flatten/Pronation:
- Frederick, E. C., & Hagy, J. L. (1986). Factors affecting peak vertical ground reaction forces in running. International journal of sport biomechanics, 2(1), 41-49.
- DeLacerda, F. G. (1980). The relationship of foot pronation, foot position, and electromyography of the anterior tibialis musclein three subjects with different histories of shinsplints. Journal of Orthopaedic & Sports Physical Therapy, 2(2), 60-64.
- Segesser B, Nigg BM. Insertionstendinosen am Schienbein, Achillodynie und Ueberlastungsfolgen am Fuss - Aetiologie, Biomechanik, Therapeutische Möglichkeiten. Orthopade 1980; 11: 834-7
- Clement DB, Taunton JE, Smart GW. Achilles tendinitis and peritendinitis: etiology and treatment. Am J Sports Med 1984; 12: 179-84
- Dhaher, Y. Y., Tsoumanis, A. D., Houle, T. T., & Rymer, W. Z. (2005). Neuromuscular reflexes contribute to knee stiffness during valgus loading. Journal of neurophysiology, 93(5), 2698-2709.
- Bahlsen AH. The etiology of running injuries: a longitudinal, prospective study . Calgary: University of Calgary, 1993: 23-67
- Basmajian JV, Stecko G. The role of muscles in arch support of the foot. J Bone Joint Surg 1963;45A: 1184-90
- Mizel MS, Temple HT, Scranton PE II, Gellman RE, Hecht PJ, Horton GA, et al. Role of the peroneal tendons in the production of the deformed foot with posterior tibial tendon deficiency.
- Dyal CM, Feder J, Deland JT, Thompson FM. Pes planus in patients with posterior tibial tendon insufficiency: asymptomatic versus symptomatic foot. Foot Ankle Int 1997;18: 85-8.
- Pohl MB, Rabbito M, Ferber R. The role of tibialis posterior fatigue on foot kinematics during walking. Journal of Foot and Ankle Research 2010 3:6
- Mosier SM, Pomeroy G, Manoli A II. Pathoanatomy and aetiology of posterior tibial tendon dysfunction. Clin Orthop Rel Res 1999;365:12-22.
- Becker, James. "Towards an Understanding of Prolonged Pronation: Implications for Medial Tibial Stress Syndrome and Achilles Tendinopathy." (2013).
- Dos Reis, A. C., Correa, J. C. F., Bley, A. S., Rabelo, N. D. D. A., Fukuda, T. Y., & Lucareli, P. R. G. (2015). Kinematic and Kinetic Analysis of the Single-Leg Triple Hop Test in Women With and Without Patellofemoral Pain. journal of orthopaedic & sports physical therapy, 45(10), 799-807.
Foot Turn Out:
- Souza, R. B., Hatamiya, N., Martin, C., Aramaki, A., Martinelli, B., Wong, J., & Luke, A. (2015). Medial and lateral heel whips: prevalence and characteristics in recreational runners. PM&R, 7(8), 823-830.
- Winslow, J., & Yoder, E. (1995). Patellofemoral pain in female ballet dancers: correlation with iliotibial band tightness and tibial external rotation. Journal of Orthopaedic & Sports Physical Therapy, 22(1), 18-21.
- Andrews, M., Noyes, F. R., Hewett, T. E., & Andriacchi, T. P. (1996). Lower limb alignment and foot angle are related to stance phase knee adduction in normal subjects: a critical analysis of the reliability of gait analysis data. Journal of orthopaedic research, 14(2), 289-295.
Knees Bow In:
- Hewett, T. E., Myer, G. D., Ford, K. R., Heidt, R. S., Colosimo, A. J., McLean, S. G., & Succop, P. (2005). Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes A prospective study. The American journal of sports medicine, 33(4), 492-501.
- Bell, D. R., Padua, D. A., & Clark, M. A. (2008). Muscle strength and flexibility characteristics of people displaying excessive medial knee displacement. Archives of physical medicine and rehabilitation, 89(7), 1323-1328.
- Andrews, M., Noyes, F. R., Hewett, T. E., & Andriacchi, T. P. (1996). Lower limb alignment and foot angle are related to stance phase knee adduction in normal subjects: a critical analysis of the reliability of gait analysis data. Journal of orthopaedic research, 14(2), 289-295.
- Dos Reis, A. C., Correa, J. C. F., Bley, A. S., Rabelo, N. D. D. A., Fukuda, T. Y., & Lucareli, P. R. G. (2015). Kinematic and Kinetic Analysis of the Single-Leg Triple Hop Test in Women With and Without Patellofemoral Pain. journal of orthopaedic & sports physical therapy, 45(10), 799-807.
- Noehren, B., Scholz, J., Davis, I. (2011) The effects of real-time gait retraining on hip kinematics, pain, and function in subjects with patellofemoral pain syndrome. Br Journal of Sports Medicine. 45:691-696
- Ireland, ML., Wilson, JD., Ballantyne, BT., Davis, IM. (2003). Hip Strength in Females With and Without Patellofemoral Pain. J Orthop Sports Phys Ther 2003. 33: 671-676
- Noehren B, Hamill J, Davis I. Prospective Evidence for a Hip Etiology in Patellofemoral Pain. Medicine & Science in Sports & Exercise. 2013;45(6):1120–1124.
- Smith, J. A., Popovich, J. M., & Kulig, K. (2014). The influence of hip strength on lower limb, pelvis, and trunk kinematics and coordination patterns during walking and hopping in healthy women. Journal of Orthopaedic & Sports Physical Therapy, (Early Access), 1-23.
- Souza, R. B., & Powers, C. M. (2009). Predictors of hip internal rotation during running an Evaluation of hip strength and femoral structure in women with and without patellofemoral pain. The American journal of sports medicine, 37(3), 579-587.
- Bolgla, L. A., Malone, T. R., Umberger, B. R., & Uhl, T. L. (2008). Hip strength and hip and knee kinematics during stair descent in females with and without patellofemoral pain syndrome. journal of orthopaedic & sports physical therapy, 38(1), 12-18
- Bolgla, L. A., & Uhl, T. L. (2005). Electromyographic analysis of hip rehabilitation exercises in a group of healthy subjects. Journal of Orthopaedic & Sports Physical Therapy, 35(8), 487-494.
- Ramskov, D., Barton, C., Nielsen, R. O., & Rasmussen, S. (2015). High Eccentric Hip Abduction Strength Reduces the Risk of Developing Patellofemoral Pain Among Novice Runners Initiating a Self-Structured Running Program: A 1-Year Observational Study. journal of orthopaedic & sports physical therapy, 45(3), 153-161
- Snyder, K. R., Earl, J. E., O’Connor, K. M., & Ebersole, K. T. (2009). Resistance training is accompanied by increases in hip strength and changes in lower extremity biomechanics during running. Clinical Biomechanics, 24(1), 26-34
- Willson JD, Lower extremity strength and mechanics during jumping in women with patellofemoral pain, Journal of Sports Rehabilitation, 2009 Feb; 18(1), 79-90
- De Marche Baldon R, Eccentric Hip Muscle Function in Females With and Without Patellofemoral Pain Syndrome, Journal of Athletic Training, 2009; 44(5): 490-496
- Bell, D. R., Vesci, B. J., DiStefano, L. J., Guskiewicz, K. M., Hirth, C. J., & Padua, D. A. (2012). Muscle activity and flexibility in individuals with medial knee displacement during the overhead squat. Athletic Training and Sports Health Care, 4(3), 117-125.
Knees Bow Out:
- Sharma, L., Song, J., Felson, D. T., Shamiyeh, E., & Dunlop, D. D. (2001). The role of knee alignment in disease progression and functional decline in knee osteoarthritis. Jama, 286(2), 188-195.
- Brouwer, G. M., Van Tol, A. W., Bergink, A. P., Belo, J. N., Bernsen, R. M. D., Reijman, M., … & Bierma‐Zeinstra, S. M. A. (2007). Association between valgus and varus alignment and the development and progression of radiographic osteoarthritis of the knee. Arthritis & Rheumatism, 56(4), 1204-1211.
- Foroughi, N., Smith, R., & Vanwanseele, B. (2009). The association of external knee adduction moment with biomechanical variables in osteoarthritis: a systematic review. The Knee, 16(5), 303-309.
- Andrews, M., Noyes, F. R., Hewett, T. E., & Andriacchi, T. P. (1996). Lower limb alignment and foot angle are related to stance phase knee adduction in normal subjects: a critical analysis of the reliability of gait analysis data. Journal of orthopaedic research, 14(2), 289-295.
- Barrios, J. A., Crossley, K. M., & Davis, I. S. (2010). Gait retraining to reduce the knee adduction moment through real-time visual feedback of dynamic knee alignment. Journal of biomechanics, 43(11), 2208-2213.
Studies Demonstrating Impairments Increase the Risk of Future Injury:
- Eckard, T., Padua, D., Mauntel, T., Frank, B., Stanley, L., Begalle, R., … & Kucera, K. (2018). Association between double-leg squat and single-leg squat performance and injury incidence among incoming NCAA division I athletes: A prospective cohort study. Physical Therapy in Sport.
- Hewett, T. E., Myer, G. D., Ford, K. R., Heidt, R. S., Colosimo, A. J., McLean, S. G., & Succop, P. (2005). Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes A prospective study. The American journal of sports medicine, 33(4), 492-501.
- Nadler, S. F., Malanga, G. A., Feinberg, J. H., Prybicien, M., Stitik, T. P., & DePrince, M. (2001). Relationship between hip muscle imbalance and occurrence of low back pain in collegiate athletes: a prospective study. American journal of physical medicine & rehabilitation, 80(8), 572-577.
- Ramskov, D., Barton, C., Nielsen, R. O., and Rasmussen, S. (2015). High Eccentric Hip Abduction Strength Reduces the Risk of Developing Patellofemoral Pain Among Novice Runners Initiating a Self-Structured Running Program: A 1-Year Observational Study. Journal of orthopaedic and sports physical therapy, 45(3), 153-161
- Leetun, D., Ireland, M., Willson, J., Ballantyne, B., Davis, I. (2004). Core stability measures as risk factors for lower extremity injury in athletes. Medicine and Science in Sports and Exercise, 36(6), 926-934.
- Zazulak, B. T., Hewett, T. E., Reeves, N. P., Goldberg, B., and Cholewicki, J. (2007). Deficits in neuromuscular control of the trunk predict knee injury risk. The American journal of sports medicine, 35(7), 1123-1130.
- Nadler, S., Wu, K., Galski, T., Feinberg, J. (1998). Low back pain in college athletes: a prospective study correlating lower extremity overuse or acquired ligamentous laxity with low back pain. Spine, 23(7), 828 – 833.
© 2019 Brent Brookbush
Questions, comments and criticisms welcome and encouraged -