Research Review: The thoracolumbar fascia: anatomy, function and clinical considerations
By Erik Korzen DC, NASM-CES, Acupuncturist
Edited by Brent Brookbush DPT, PT, COMT, MS, PES, CES, CSCS, ACSM H/FS
Original Citation: Willard, F.H., Vleeming, A., Schuenke, M.D., Danneels, L., Schleip, R. The thoracolumbar fascia: anatomy, function and clinical considerations. Journal of Anatomy, 2012. 221, 507-536. Full Article
Why is this relevant?: The thoracolumbar fascia (T/L fascia) is a complex network of myofascial structures that exist to stabilize the lumbopelvic area and provide a connection between the extremities and trunk. This study includes anatomical and histologic examination of the passive and active structures associated with the T/L fascia as well as the embryologic origin of many relevant structures. The researchers performed an extensive review of the current, and sometimes conflicting, evidence surrounding the T/L fascia. This includes histologic examination, innervation, biomechanics and clinical considerations. The findings of this study imply that the T/L fascia is more realistically based on a 2 layer model that receives proprioceptive and nociceptive innervation. Additionally, the findings indicate that the T/L fascia can transmit tension and therefore assist in stabilizing the lumbar spine and sacroiliac joints.
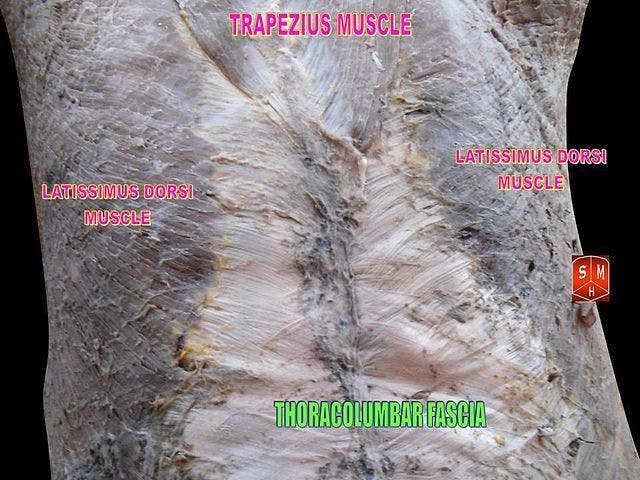
By Anatomist90 - Own work, CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=17900177; Thoracolumbar fascia. Notice the lighter colored band of tissue. This is the fascia.
Study Summary
| Study Design | Review |
| Level of Evidence | Level of Evidence III - Evidence from non-experimental descriptive studies, such as comparative studies, correlation studies, and case-control studies |
| Subject Demographics | Not Applicable |
| Outcome Measures | T/L Fascia Anatomy, Histology, Innervation, Biomechanics, Clinical Relevance were all considered in this review article Alphabetical Abbreviations used throughout the article:
|
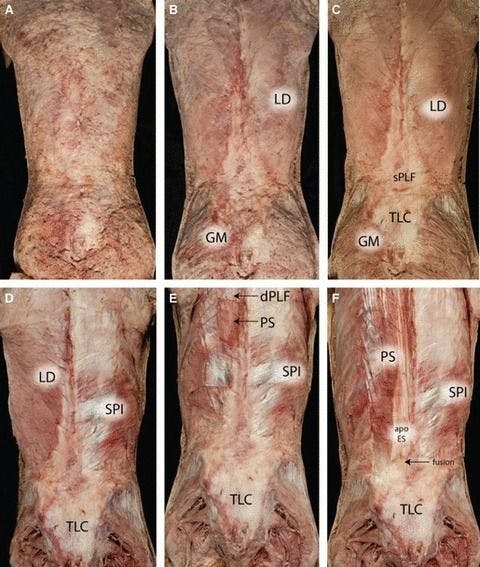
| Results | The TLF, similar to other fascial structures, is composed of irregularly situated collagen fibers that will withstand stress in multiple directions. There are clearly multiple layers of the TLF, although there is some debate on whether this is a 3 layer structure or a 2 layer structure. Regardless, the TLF is composed of aponeurotic and fascial planes that unite around the paraspinal musculature. The latissimus dorsi (LD) and serratus posterior inferior (SPI) contribute to the posterior layer of the thoracolumbar fascia (PLF) via their aponeurotic attachments. In the lower lumbar region the erector spinae are completely surrounded by the dense aponeurosis. Below L5 vertebra there is a very thick aponeurotic structure that attaches laterally to the iliac crest near the posterior superior iliac spine (PSIS) and terminates at the sacrotuberous ligament (STL). The structure termed "middle layer of the thoracolumbar fascia (MLF)" is actually composed of the paraspinal retinacular sheath (PRS) and the aponeurosis of the transverse abdominis (TrA) as these structures fuse with the epimysium of the quadratus lumborum (QL). The structure described as the PRS essentially represents the epaxial fascial sheath that the paraspinal muscles formed during embryogenesis. The posterior layer of the thoracolumbar fascia (PLF) is a structure that can be divided into 3 sublayers, 2 of which derive from the epimysium and aponeurosis of the LD. The LD muscle itself contains fibers of varying angles, from horizontal more superiorly and 20-40° more inferiorly. The SPI contains fibers that attach to the aponeurosis of the LD more medially. An interesting finding is that both the LD and SPI are innervated by ventral rami which indicate that neither of these muscles are epaxial in origin. During embryogenesis the LD and SPI must migrate posteriorly to their final, functional position. The MLF is a structure that exists between the QL and paraspinal muscles and has been suggested as a primary connection between abdominal tension and the lumbar spine. The lower border of the MLF is actually the iliolumbar ligament and iliac crest. Apparently the MLF is slightly thicker than the PLF and contains attachments for the TrA and IO muscles. There is also a relatively strong connection of the MLF to the transverse processes in the lumbar spine. Based on previous research, the MLF contains portions of both hypaxial and epaxial origins. An additionally complex structure is termed the lateral raphe which exists at the junction of the hypaxial and epaxial muscles, forming the lateral border of the PRS. This structure, along with the PRS and aponeurosis of the TrA creates the lumbar interfascial triangle (LIFT). Innervation: There appears to be a correlation between the innervation of muscles and fascia in similar areas which has led to the proposal of ‘fasciotomes’. This term implies that fascia contains segmentally innervated patterns similar to the myotomes. Unfortunately, histologic evidence has yet to fully support this notion. An intriguing finding regarding innervation is that fascia seems to contain a high density of sympathetic fibers. Furthermore, the TLF contains Golgi, Pacini and Ruffini endings, indicating a potential proprioceptive role. The proprioceptive role of the spinal facet joints appears to occur only during larger joint movements and thus the TLF could experience a sufficient stretch to stimulate these nerve endings. It has been determined that the transverospinalis group of muscles, such as the rotatores and multifidi, contain a high density of muscle spindles and therefore could function more proprioceptively than initiating movements. Regarding the nociceptive role of the TLF, there are substance P-positive fibers in the superficial layer but are not present in the intermediate and deep layers. Biomechanical: The lumbosacral area is a combination of the spine and lower extremities which are united by the TLC of fascia and aponeuroses. There is also an obvious myofascial connection between the lumbosacral region and the upper extremities. Strain-energy is a term used to described how the TLF deforms during movements and assists in lifting loads by reducing muscle contraction requirements. With respect to moment arms, the TLF is positioned to create large extensor moments with minimal compressive forces on the spinal column. The increase of intra-abdominal pressure (IAP) is largely due to torso muscular contraction, namely the TrA which clearly contains attachments to the TLF. “The TrA generated a rise in IAP, and was demonstrated to be fast and of sufficient magnitude to increase the stability of the lumbar spine prior to the contraction of torque-producing muscles.” The paraspinal muscles are contained within the previously mentioned PRS and their radial expansion can be limited by the TLF. Some important extremity muscles include the LD and gluteus maximus (GM). When traction is applied to the GM there is a contralateral displacement of the TLF. Due to it’s attachment to the sacrotuberous ligament (STL), the biceps femoris tendon can cause displacement of the deep layer approximately at L5-S1. The PLF can play a significant role in transferring forces between the spine, pelvis and lower extremities. Based on fiber orientation, the TrA functions to pull the ilium towards each other thereby stabilizing the 2 surfaces of the sacroiliac joint (SIJ). |
| Conclusions | Manual medicine, or myofascial treatments, may effect the fascia via sympathetic nerves and is therefore feasible that the stimulation of intrafascial sympathetic afferents may trigger modifications in global autonomic nervous system tone, as well as in local circulation and matrix hydration (Schleip, 2003). Proprioceptive innervation is equally important because studies suggest that subjects with low back pain have a reduction in lumbosacral proprioception. There are 3 potential nociceptive findings: 1: microinjuries and resulting irritation of nociceptive nerve endings in the TLF may lead directly to back pain, 2: tissue deformations due to injury, immobility or excessive loading could also impair proprioceptive signaling, which by itself could lead to an increase in pain sensitivity via an activity-dependent sensitization of wide dynamic range neurons, 3: irritation in other tissues innervated by the same spinal segment could lead to increased sensitivity of the TLF, which would then respond with nociceptive signaling, even to gentle stimulation. Biomechanically, the TrA produces spinal stability due to increased IAP created via it's contraction. Furthermore, with the PSIS of the ilia anchored in place by the TLC, contraction of the TrA and, to a lesser degree the IO, would be able to compress the sacroiliac joint. There is also sufficient evidence to suggest that the contralateral gluteus maximus (GM) and LD create forces perpendicular to the SIJ and spinal facet joints, leading to tension transfer and stability. Rotation of the trunk is mainly a function of the abdominal muscles. However, a counter-muscle sling in the back, in contrast to the abdominal sling, helps to preclude deformation of the spine. Rotation against increased resistance will activate the posterior oblique sling of GM and LD (Vleeming & Stoeckart, 2007). |
| Conclusions of the Researchers | The most common terminology for the TLF is derived from the 3 layer model, although the 2 layer model is more realistic. There is clear evidence that the TLF contains, to a certain degree, both proprioceptive and nociceptive innervation. This finding can then be extrapolated to relate the TLF and low back pain. The TrA and other muscles can create tension that is distributed via the TLF to stiffen the lumbar spine and stabilize the SIJ. |
Thoracolumbar Fascia
Commentary:
Why is this study important?
The complexity of the thoracolumbar fascia (TLF) results in varying opinions on the biomechanical and neurologic involvement in practical applications. The authors of this study performed a thorough review of existing research regarding the TLF, detailing the functional anatomy, and also considered histologic and embryologic evidence. Further, use this comprehensive review in conjunction with basic sciences, to suggest potential practical application. The TLF is a rather elaborate structure that may play a in proprioception, our perception of low back pain, lumbar stability and affect both upper and lower extremity motion.
How does it affect practice?
While the TLF is a structure that is often referred to by human movement professionals (especially, with the increase in research published on fascia), its function has been an area of debate. After careful review, it may be concluded that the TLF is myofascial connection between the torso and the extremities, and may function to transmit forces between muscles that insert into it. The TLF, also plays a role in increasing intra-abdominal pressure and providing stability to the lumbosacral spine and sacroiliac joints. Last, there are both proprioceptive and nociceptive nerve ending present in the TLF which may imply a role in afferentation, specifically pain and proprioception.
Interventions with the intent of affecting the lumbo pelvic hip complex, should consider the influence the TLF has on motion and sensation, as well as, all of the relationships that the TLF implies. For example, activation of the commonly under-active gluteus maximus and gluteus medius muscles, will alter tension in the TLF, which may affect the muscles of the trunk (including the TvA ), the joints of the lumbar spine, proprioception and the stimulation of nociceptors present in the TLF and lumbar region. The same example, could be give for the latissimus dorsi . If we look at the affect motion has on the TLF, we may be able to implicate that an increase in intra-abdominal pressure during many lifts will increase tension in the TLF, which may result in an increase in TvA activity, enhanced stability of the lumbar spine, and aid in transferring force between the lower and upper extremities (gluteus maximus and latissimus dorsi ) - important for sports performance?
How does it relate to Brookbush Institute Content?
Because the TLF is invested by and may affect so many muscles and joints, it is considered in all of the Brookbush Institute predictive models of postural dysfunction - lumbopelvic-hip complex (LPHCD) , upper body dysfunction (UBD) and lower body dysfunction (LLD) can all be effected by abnormalities in the function of this tissue. Practical applications of these considerations include release and lengthening of the latissimus dorsi and erector spinae , mobilization of the spine and SIJ , activation of the gluteus medius and gluteus maximus , integration of the posterior oblique subsystem (POS) , and potentially affecting the posterior oblique subsystem through taping techniques . In the future, the Brookbush Institute will need to do more consideration of techniques that directly affect the TLF including manual release and instrument assisted soft tissue mobilization.
The videos below demonstrate progressions for Posterior Oblique Subsystem Integration (Latissimus Dorsi, Thoracolumbar Fascia, Gluteus Maximus and Gluteus Medius)
Bibliography
Willard, F.H., Vleeming, A., Schuenke, M.D., Danneels, L., Schleip, R. The thoracolumbar fascia: anatomy, function and clinical considerations. Journal of Anatomy, 2012. 221, 507-536.
© 2016 Brent Brookbush
Questions, comments, and criticisms are welcomed and encouraged -