Research Review: Unilateral Hip Rotation Range of Motion Asymmetry in Patients With Sacroiliac Joint Regional Pain
By Amy Martinez DPT, PT
Edited by Brent Brookbush DPT, PT, COMT, MS, PES, CES, CSCS, ACSM H/FS
Original Citation: Cibulka, M. T., Sinacore, D. R., Cromer, G. S., & Delitto, A. (1998). Unilateral hip rotation range of motion asymmetry in patients with sacroiliac joint regional pain. Spine, 23(9), 1009-1015. - ABSTRACT
Introduction: Research has demonstrated a correlation between low back pain (LBP), hip external rotation greater than internal rotation, and asymmetries in hip range of motion (ROM) (1 - 3). Additionally, research has demonstrated asymmetrical external rotation ROM in individuals with sacrociliac joint (SIJ) dysfunction (4 - 6). Prior research has demonstrated a correlation between SIJ pain and a relative tilt of a pelvic innominate (7 - 8); however, these studies did not make an attempt to also correlate changes in hip ROM. This 1998 study by American researchers demonstrates that hip external rotation ROM is asymmetrical and significantly greater on the side of the posteriorly inomminate tilt (PIT) in individuals with LBP and/or SIJ pain. These findings suggest that hip range of motion and relative tilt of the pelvic innominate should be assessed in individuals exhibiting symptoms of LBP and/or SIJ pain.
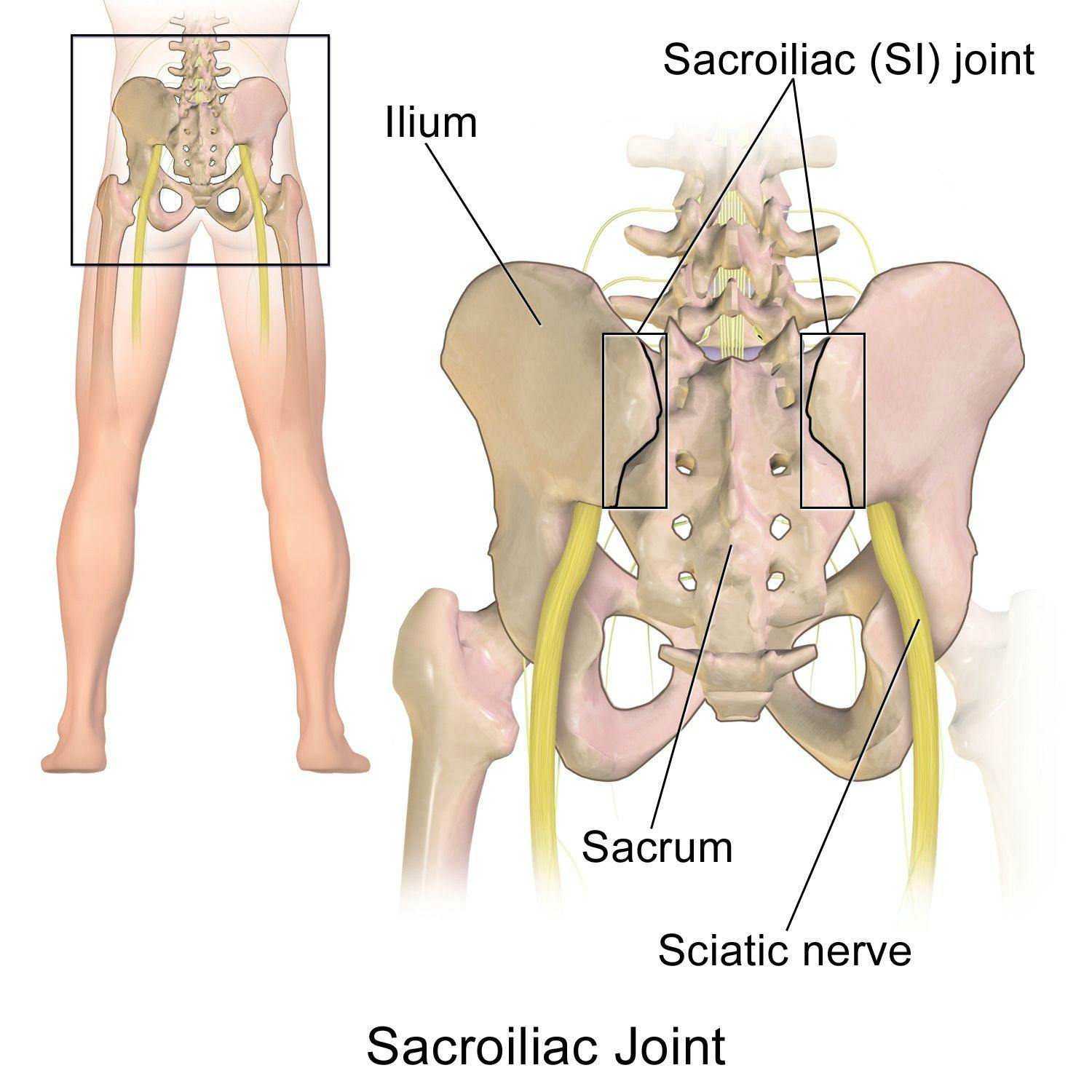
Sacroiliac Joint. (Image: BruceBlaus - own work, cc-by-3.0, https://commons.wikimedia.org/wiki/File:Sacroiliac_Joint.png)
Study Summary
| Study Design | Cross-sectional, observational study |
| Level of Evidence | Level III - Evidence from non-experimental descriptive studies, such as comparative studies, correlation studies and case-control studies |
| Participant Characteristics | Demographics
Inclusion Criteria:
Exclusion Criteria:
|
| Methodology |
|
| Data Collection and Analysis | Hip Rotation ROM was analyzed with two multivariate analysis of variance (MANOVA) tests:
Intra-rater Reliability
|
| Outcome Measures |
|
| Results | All Participants
Sacroiliac Joint Regional Pain
Intra-rater Reliability
|
| Our Conclusions | The findings of this study reinforce the asymmetry in hip ROM and posterior rotation of the innominate on the side of reduced hip IR as part of the altered movement patterns described in the Brookbush Institute’s predictive models of Lumbo Pelvic Hip Complex Dysfunction (LPHCD) and Sacroiliac Joint Dysfunction (SIJD). |
| Researchers' Conclusions | This study demonstrates that participants with LBP exhibit greater external than internal hip rotation ROM. In participants who had signs of sacroiliac joint regional pain, there was significantly more external hip rotation ROM on the side of the posteriorly tilted innominate. These findings imply a compensation pattern, and that unilateral hip rotation ROM asymmetry in patients with LBP may also be related to sacroiliac joint regional pain. |

Goniometry of hip external rotation in a prone position. (Image: Courtesy of www.BrentBrookbush.com)
How this study contributes to the body of research:
This study on 100 LBP patients investigated hip rotation ROM, signs of SIJ regional pain, side of relative posterior innominate tilt, and inter-rater reliability of all tests. Prior studies have demonstrated, individuals with low back pain (LBP) exhibit more hip external rotation than internal rotation range of motion (ROM) bilaterally; however, those who exhibit sacroiliac (SI) joint regional pain exhibit asymmetry in external rotation ROM (1-6). Unique to this study, researchers demonstrated that individuals with SI joint regional pain, exhibited more hip external rotation ROM on the side of the posteriorly innominate tilt (PIT). This study may imply a compensation pattern, and/or correlations between LBP, SIJ pain, relative PIT on one side, and asymmetry in hip rotation ROM (specifically more hip external rotation). Note, this study also demonstrated good inter-rater reliability for all tests.
How the Findings Apply to Practice:
The findings of this study suggest that in individuals with sacroiliac (SI) joint regional pain, a unilateral asymmetry in hip external rotation range of motion (ROM) is associated with a posterior innominate (PI) tilt. This suggests that individuals with LBP and/or SIJ should be assessed for asymmetries during functional activity, asymmetries in hip ROM, posterior superior iliac spine height, and potentially SIJ stiffness. Further, the human movement professional should be prepared with techniques to address any assessed issues.
The study had many methodological strengths, including:
- Researchers were blinded to participants’ performance on SIJ and goniometric assessments, enhancing the validity of data collection and minimizing tester bias.
- Intra-rater reliability was calculated through weighted K and intra-class correlation coefficients (ICCs), demonstrating significance and reliability for the data collected.
- The SIJ special test methods were clearly described in the study, enhancing clinical applicability.
- Researchers established a minimum observable difference of 2.54 cm (1 inch) for SIJ tests, enhancing the reliability of the results.
Weaknesses that should be noted prior to clinical integration of the findings include:
- A 'gold standard' for detecting movement dysfunction of the SIJ, and SIJ tests rely on palpation and the examiner's skills; this limits test reliability. (Note: the minimum of 1 inch difference mentioned above would aid in improving reliability)
- A control group was not used for comparison in this study, introducing a detection bias in the results.
- Participants completed a pain drawing to describe their pain, but this process was not described in detail; this may limit the ability to compare or replicate this study.
- The results of hip ROM values were presented in graph format. Providing objective numerical data would enhance interpretation of the results and comparison between similar studies.
How the study relates to Brookbush Institute Content:
The Brookbush Institute has developed predictive models of postural dysfunction based on evidence of common tissue changes (muscle, joint, fascia and nerve) to aid human movement professionals in selecting optimal assessments, manual interventions and exercise. The Lumbo Pelvic Hip Complex Dysfunction (LPHCD) and Sacroiliac Joint Dysfunction (SIJD) models note changes in hip mobility that are consistent with the findings of this study, including a decrease in hip internal rotation compared to external rotation, and potential asymmetry between right and left hip ROM.
The following videos illustrate common assessment techniques for the LPHCD and SIJD :
Overhead Squat Assessment: Sign Clusters – Lumbo Pelvic Hip Complex Dysfunction
Overhead Squat Assessment: Sign Clusters – Asymmetrical Weight Shift
Goniometry: Hip external rotation in prone
Goniometry: Hip internal rotation in prone
Stork Test: Special Test for SIJ Motion
Bibliography:
- Barbee Ellison, J., Rose, S. J., & Sahrmann, S. A. (1990). Patterns of hip rotation range of motion: a comparison between healthy subjects and patients with low back pain. Physical Therapy, 70(9), 537-541.
- Mellin, G. (1988). Correlations of hip mobility with degree of back pain and lumbar spinal mobility in chronic low-back pain patients. Spine, 13(6), 668-670.
- Chesworth, B. M., Padfield, B. J., Helewa, A., et al. (1994). A comparison of hip mobility in patients with low back pain and matched healthy subjects. Physiother Can, 46, 267-274.
- LaBan, M. M., Meerschaert, J. R., Taylor, R. S., & Tabor, H. D. (1978). Symphyseal and sacroiliac joint pain associated with pubic symphysis instability. Archives of physical medicine and rehabilitation, 59(10), 470-472.
- Cibulka, M. T. (1992). The treatment of the sacroiliac joint component to low back pain: a case report. Physical therapy, 72(12), 917-922.
- Fowler, C. (1986). Muscle energy techniques for pelvic dysfunction. Modern Manual Therapy of the Vertebral Column. Edinburgh, Scotland: Churchill Livingstone, 805-14.
- Cibulka, M. T., Delitto, A., & Koldehoff, R. M. (1988). Changes in innominate tilt after manipulation of the sacroiliac joint in patients with low back pain: an experimental study. Physical Therapy, 68(9), 1359-1363.
- Cummings, G., Scholz, J. P., & Barnes, K. (1993). The effect of imposed leg length difference on pelvic bone symmetry. Spine, (18), 368-368.
- Waddell, G., McCullock, J.A., Kummel, E., et al. (1980). Non-organic physical signs in low-back pain. Spine, (5), 117-125.
© 2018 Brent Brookbush
Questions, comments and criticisms are welcomed and encouraged.