Deltoids
Integrated functional anatomy of the anterior, middle, and posterior deltoid. Attachments, nerves, palpation, joint actions, arthrokinematics, fascia, triggerpoints, and behavior in postural dysfunction. Common exercises, foam rolling, and stretches for the deltoid/shoulder muscles.
Course Description: Deltoids
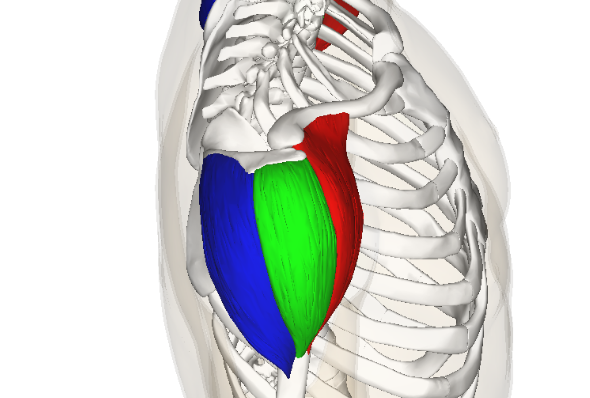
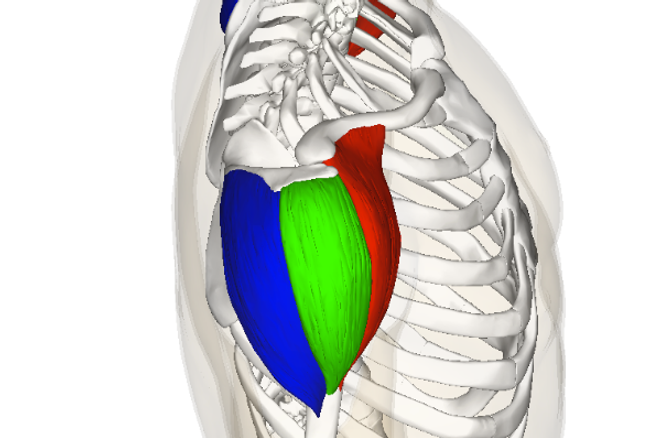
This course describes the anatomy and integrated function of the deltoid muscle (a.k.a. the delts, shoulder muscles, or referenced individually as the anterior deltoid or front deltoid, posterior deltoid or rear deltoid, and the middle deltoid, medial deltoid, or lateral deltoid). The deltoid muscle originates on the acromion process of the scapula (shoulder blade) and the lateral 1/3 of the clavicle, all three divisions of the deltoid muscle insert into the deltoid tuberosity, and all divisions are innervated by the axillary nerve. The deltoids are the most superficial muscles of the shoulder and are composed of a relatively even proportion of type I muscle fibers and type II muscle fibers; however, these proportions can vary considerably. The deltoid muscle crosses the shoulder joint (glenohumeral joint) and contributes to shoulder joint actions. The anterior deltoid is the primary shoulder flexor and will contribute to shoulder horizontal adduction and shoulder internal rotation. The middle deltoid (lateral deltoid) is the primary shoulder abductor. And, the posterior deltoid (rear delt) is the primary shoulder horizontal abductor and will contribute to shoulder extension and shoulder external rotation. This course also describes the role of the deltoid muscles in glenohumeral arthrokinematics, fascial integration, postural dysfunction, and subsystem integration. Sports medicine professionals (personal trainers, fitness instructors, physical therapists, massage therapists, chiropractors, occupational therapists, athletic trainers, etc.) must be aware of the integrated function of the deltoids for the detailed analysis of human movement, and the development of sophisticated exercise programs and therapeutic (rehabilitation) interventions. Further, this course is essential knowledge for future courses discussing injury prevention and physical rehabilitation (e.g. deltoid pain, shoulder joint pain, “shoulder blade pain,” “uneven shoulder height,” axillary nerve damage, rotator cuff injury, shoulder impingement syndrome, scapula dyskinesis), the synergistic function of the deltoid muscles (e.g. during shoulder exercises like an upright row or a lateral raise the middle deltoid abducts the humerus in synergy with the supraspinatus of the rotator cuff), and deltoid exercises and techniques for enhancing sports performance (e.g. training the deltoids with shoulder exercises to optimize stability, strength, power, and shoulder hypertrophy, etc.).
Brookbush Institute’s most recommended techniques for the Deltoids (see videos below):
- Release: Posterior Shoulder Foam Rolling
- Stretch: Posterior Shoulder (Sleeper) Stretch
- Conditioning: Shoulder and Pressing Progressions
Study Guide: Anatomy of the Deltoids
Introduction to the Deltoids
3 sub-categoriesDeltoid Muscle Actions
2 sub-categoriesFascial Integration
1 sub-categoryPostural Dysfunction & the Deltoids
Exercises and Techniques for the Deltoid Muscles
3 sub-categoriesBibliography
© 2024 Brookbush Institute. All rights reserved.